Pedro Lylyk a, b, Juan Cirio a, b, Carlos Toranzo a, b, Eleonora Aiello c, Juan Valencia d, Daniela Paredes-Fernández e,∗
a Instituto Médico ENERI – Equipo de Neurocirugía Endovascular y Radiología Intervencionista, Buenos Aires, Argentina
b Stroke Unit, Clinica ́ La Sagrada Familia, Buenos Aires, Argentina
c Independent Consultant, Buenos Aires, Argentina
d Health Economics, Policy and Reimbursement, Medtronic Latin-America, USA
e Health Economics, Policy and Reimbursement, Medtronic South Latin-America, 532 Rosario Norte Street, Las Condes, Chile
Abbreviations: AR$, Argentinian Peso; BIA, Budget-impact analysis; EMP, Empresas de Medicina Prepaga; ICER, Incremental cost-effectiveness ratio; IV-tPA, Intra venous tissue plasminogen activator; mRS, Modified Rankin Scale; MT, Mechanical thrombectomy; NMB, Net monetary benefit; OS, Obras Sociales; QALY, Quality – adjusted life years; QOL, Quality of life; USD, United States dollar; WTP, Willingness to pay.
∗ Corresponding author. E-mail address: [email protected] (D. Paredes-Fernández).
La trombectomía mecánica (TM) después de la trombolisis IV con tPA (IV-tPA) en un ataque cerebro-vascular (ACV) debido a una oclusión de gran vaso cerebral, es efectiva tanto clínica como económicamente. En este estudio analizamos el costo y el impacto económico de la TM luego de IV-tPA, tanto para nuestras Obras Sociales como para las Empresas de Medicina Pre-pagas. Para tal fin, adaptamos publicaciones internacionales previas de la TM asociada a IV-tPA al contexto Argentino, para conocer nuestro costo-efectividad del tratamiento combinado en el ACV por oclusión de gran vaso.
ABSTRACT
Objectives: Mechanical thrombectomy (MT) after intravenous thrombolysis (IV-tPA) is an effective and cost-saving treatment for stroke due to large vessel occlusion. However, rates of MT use are low in Argentina. This study was designed to estimate the economic value and the budget impact of incorporating MT after thrombolysis, simulating scenarios from Argentinian compulsory social health insurance (Obras Sociales) and private insurances (Empresas de Medicina Prepaga).
Materials and methods: We adapted a previously published cost-utility and budget-impact (CUA and BIA) model to the Argentinian setting. The CUA was carried out for a lifetime horizon with efficacy inputs from the SWIFT PRIME clinical trial. For seven possible health states, we identified local costs (Argentinian Pesos AR$), utility (QALY), and transition/distribution probabilities (5% discounted rate) and performed deterministic and probabilistic sensitivity analyses. The BIA was based on a six-step approach and a static
model for a five-year horizon, and two scenarios (staggered growth and no growth).
Results: Despite higher incremental procedure costs, IV-tPA and MT was dominant over IV-tPA alone (AR$1,049,062 overall savings). Cost-effectiveness remained in the deterministic sensitivity analysis (100% probability of cost-effectiveness). Increased MT procedure volume resulted in savings in years three (0.96%), four (2.6%), and five (4.4%). By year five, 1,280 patients were treated with MT (versus 480) with overall savings of 1.8% (AR$817,244,417).
Conclusions: MT after IV-tPA is cost-effective in Argentina. Savings offset the incremental hospitalization and long-term costs from the third year onwards. With increased, access the superior efficacy of MT mitigates future disability and comorbidity, reducing overall expenses.
Introduction
Stroke is the leading cause of disability and the fourth leading cause of death in developed countries. In Argentina, the annual incidence of ischemic stroke for all ages has been estimated at 67.9 per 100,000 population (approximately 30,000 cases per year) with a prevalence of 834.45/100,000, or about 370,000 cases.1–3
Between 61% and 88% of all strokes are ischemic, resulting from occlusion of intracranial arteries. Of those, approximately 25% are due to large vessel occlusion (LVO).4,5
Evidence from high-quality clinical studies demonstrates that using endovascular Mechanical thrombectomy (MT) after throm bolysis with intravenous tissue plasminogen activator (IV-tPA) is highly effective in treating stroke due to LVO, reducing disability
and improving quality of life (QOL) for most of patients.6–13
Economic studies in multiple countries have established that the MT clinical efficacy translates to long-term savings in healthcare costs and resource use.14–16
However, despite the favorable clinical and economic profile of MT, its uptake in the Argentinian healthcare system has been slow. The study aimed to investigate both the cost-utility of MT from the perspective of Argentinian payers and the five-year budget impact of increasing patient access to this treatment.
Objectives
The present study was designed to quantify the economic value of IV-tPA and MT for stroke due to LVO compared to IV-tPA alone, using a previously validated economic model and adapted to the perspective of Argentinian compulsory Social Security and private prepaid health payers.15
Methods
Study design, ethics, and data analysis
This study was based on the University of York Health Economics Consortium model,15 validated and adapted to the Argentinian setting. No real-world patient data were used. No ethics approval was needed because all model inputs were derived from deidentified sources and published literature.
Construction of data models and all statistical analyses were performed using Microsoft Excel and Visual Basic.
Model inputs
A literature search was performed to identify epidemiological studies and stroke registries,17–22 published treatment consensus guidelines,23,24 and studies about costs and resource use in stroke treatment,2,25,26 specific to the Argentinian population, 2005 to present. No studies were identified that analyzed the cost effectiveness of MT or thrombolysis in Argentina. The Supplemental Online Methods includes a detailed description of model inputs and sources.
Treatment efficacy data were derived from SWIFT PRIME, an international, randomized, open-label clinical trial.
SWIFT PRIME compared the clinical efficacy of IV-tPA alone with IV-tPA and MT using the Solitaire endovascular stent retriever (Medtronic Plc, Minneapolis, Minnesota, USA) in patients with confirmed occlusions of the proximal anterior intracranial circulation and absence of large ischemic core lesions.13
SWIFT PRIME was chosen because it delivered the most comprehensive data set for the requirements of this model and, at the time the model was carried out, Solitaire (the medical device used in SWIFT PRIME) was the most utilized mechanical thrombectomy device in Argentina. Local data demonstrated results for mRS similar to those observed in SWIFT PRIME for the same time-window (within 6 h).
It is notable that the majority of SWIFT PRIME participants were selected using RAPID CT Perfusion software. This technology is available in two comprehensive stroke centers in Argentina, including Clínica Sagrada Familia, and expanding to others.
Other providers have access to MRI and disease-specific scales for out of time treatment window cases, and mechanical thrombectomy is performed by numerous other comprehensive stroke centers in major cities (e.g., Tucumán, Córdoba, Santa Fe, Buenos Aires Province, Buenos Aires City, Neuquén, Mendoza, and others).
The manufacturer validated cost data for the stent retriever device. Costs of emergency care, images, lab work, and similar services were provided by Clínica Sagrada Familia. All other input data were informed by published literature, public sources, expert opinion of neuro-interventional experts, and collaborating Social Security and Prepaid healthcare sources, which between the two of them provide coverage to 65% of the population. Costs are expressed in local currency (Argentinian Pesos; AR$) as of May 2020.
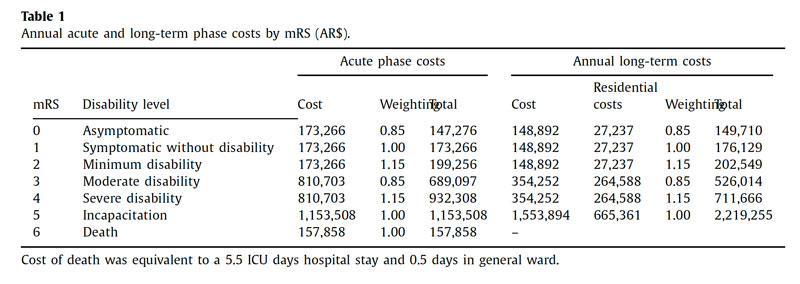
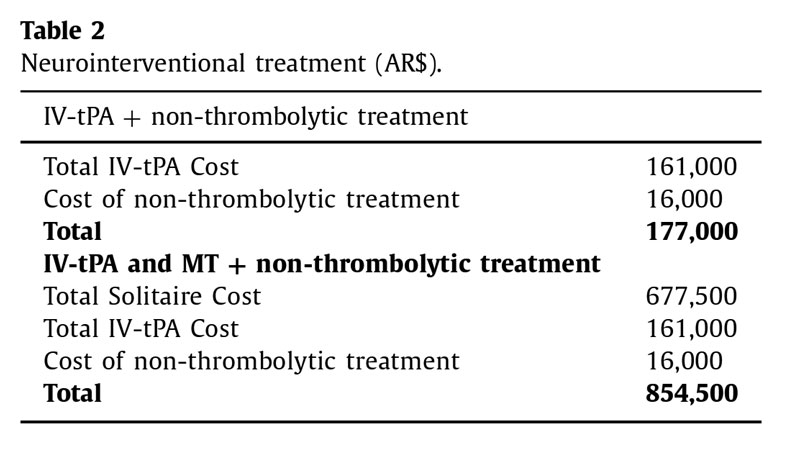
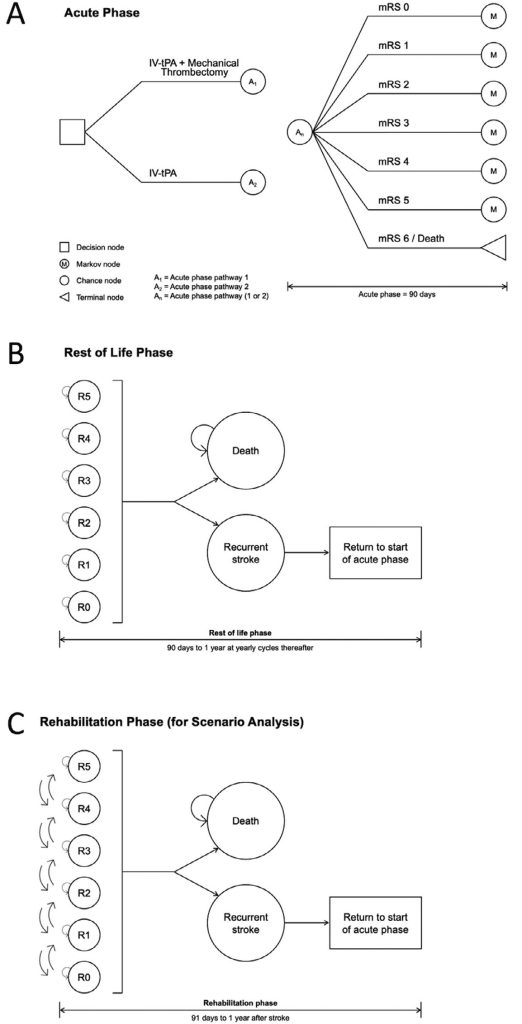
Cost-utility analysis
The model used a Markov structure divided into an acute (symptom onset through 90 days) and a “rest-of-life” (day 91 until death from any cause) phase. Patients were assigned to treatment-specific health states with an equal probability according to the distribution of modified Rankin Scale (mRS) scores observed in SWIFT PRIME (Table 1),13,24 at seven to 10 days after stroke or discharge, and again at 90 days, to allow for mid-cycle correction. A mid-cycle correction was incorporated to estimate patient transitions between health states.27 For specific costs related to neurointerventional treatments, refer to Table 2.
The model calculated total costs and quality-adjusted life-years (QALYs) for a hypothetical cohort of 1,000 patients per treatment arm, over a lifetime horizon from the onset of stroke symptoms to death. The baseline age was set at 69.4 years based on the ReNACer
registry.22
During the acute phase (Fig. 1A), patients were considered at risk for symptomatic bleeding and vasospasm.14–16 In Argentina, such events do not incur additional costs to the payer. No disutility was applied, as the impact on QOL was assumed to be reflected in
the mRS. We assumed that patients were not at risk of recurrent stroke in the acute phase.
In the base case, the rest-of-life phase (Fig. 1B) was calculated in annual cycles. The first cycle ended at one year following a patient’s stroke (275 days follow-up plus the 90-day acute post- stroke recovery phase). Patients entered the rest-of-life phase at the same mRS score at which they exited the acute phase and remained at that score until stroke recurrence or death.
The risk of recurrent stroke was applied equally across all mRS scores and the model allowed for a maximum of one recurrent stroke per patient per cycle, based on Mohan et al.28 Patients experiencing recurrent stroke re-started the model at an equal or greater mRS score. All patients continued to cycle through the model until death.
In the scenario analysis (Fig. 1C), a rehabilitation phase was introduced, encompassing the 275 days following the acute phase.
Patients could improve or worsen in mRS,28 based on evidence that post-stroke mRS scores may not stabilize until the end of the first year.29–31
The incremental cost-effectiveness ratio (ICER) and net monetary benefit (NMB) were calculated based on the discounted cumulative costs and QALYs (5% rate). Cost-effectiveness was determined relative to the willingness-to-pay (WTP) threshold. A proce-
dure was considered highly cost-effective when the ICER was equal to or less than one GDP per capita (AR$704,859/QALY). A positive NMB value indicated that IV-tPA and MT combined therapy would benefit the health system considering the WTP, with higher values
indicating more significant benefits.
Deterministic and probabilistic sensitivity analyses were performed to account for parameters’ first-order and joint uncertainty.
Budget-impact analysis
To evaluate the budget impact, on OS and EMP, of increasing MT to treat ischemic stroke due to LVO, a BIA was conducted over a 5-year horizon, based on a 6-step approach and a static model, using population, market dynamics, and cost inputs as described above and in the Supplemental Online Methods. Two scenarios were tested: the base case assumed a static MT rate of 15% over five years, and the growth scenario assumed annual growth reaching a rate of 40% MT in year five. The costs of each scenario accounted for all the resources involved in care. The model was constructed using Microsoft Excel according to best practices.32
Results
Cost-utility analysis
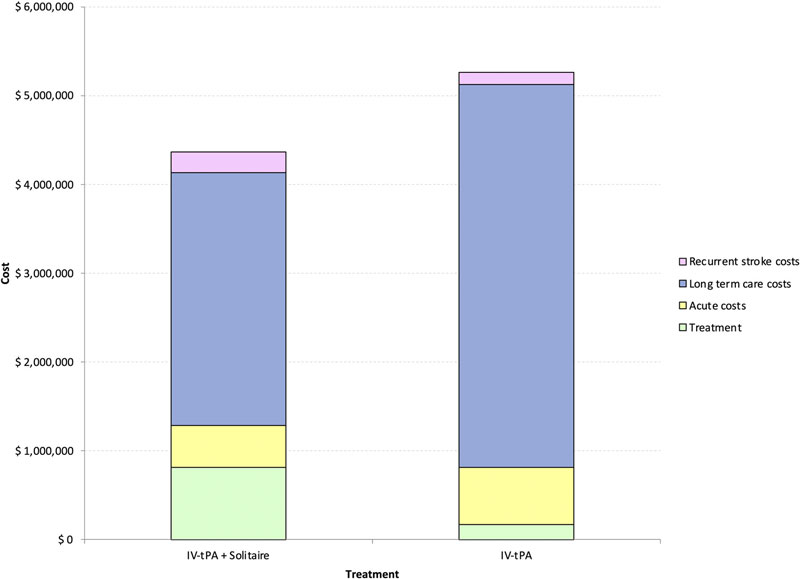
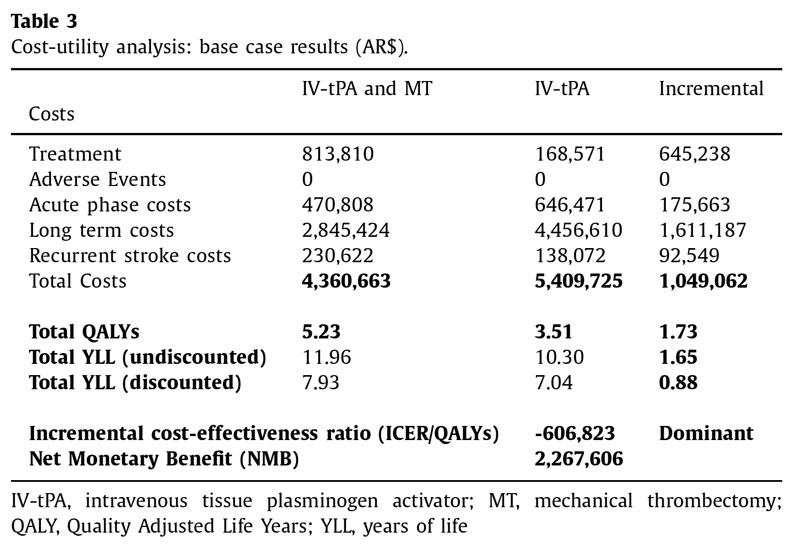
In the base case (Table 3), the model estimated the total cost of combined IV-tPA and MT therapy over the patient’s lifetime at AR$4,360,663, versus AR$5,409,725 for IV-tPA alone (AR$1,049,062 net savings; (Fig. 2). IV-tPA and MT resulted in patients being distributed toward lower levels of disability and provided more discounted years of life and QALYs (7.93 and 5.23, respectively) compared to IV-tPA alone (7.04 and 3.51, respectively). IV-tPA and MT proved to be more effective and less expensive treatments than IVt-PA alone, with a dominant (negative) ICER of AR$606,823/QALY.
In terms of NMB, a gain of AR$2,267,606 was obtained relative to the WTP threshold of one GDP per capita.
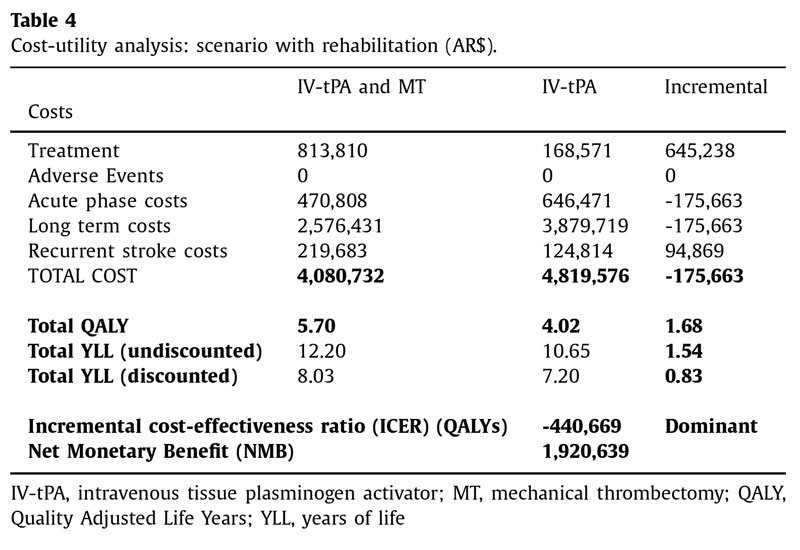
By incorporating a rehabilitation phase, IV-tPA and MT remained dominant with savings (AR$738,843) and an NMB of AR$1,920,639 compared to IV-tPA alone (Table 4).
The deterministic sensitivity analysis found that NMB grew as long-term costs, acute phase costs, health utilities, and acute phase costs increased. In contrast, the NMB decreased with increasing age at onset of stroke, the relative risk of death, and the discount rate.
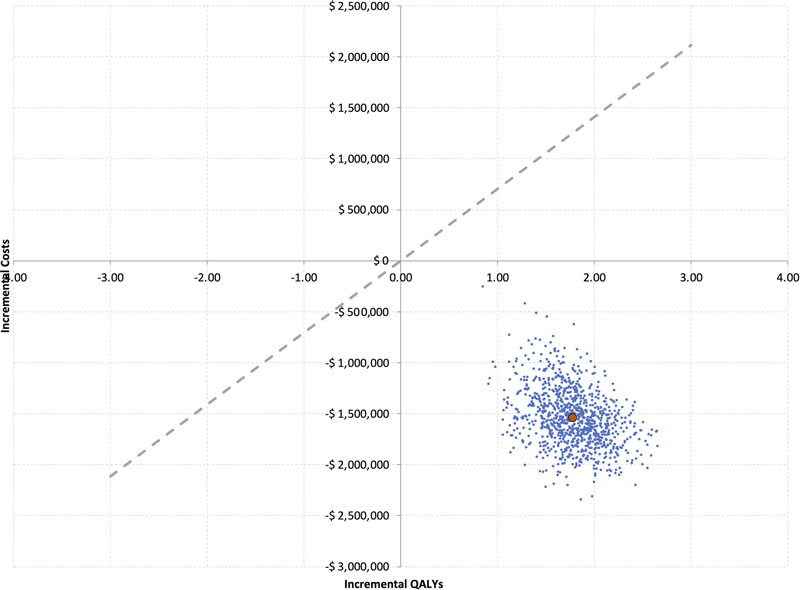
The probabilistic sensitivity analysis found that IV-tPA and MT have a 100% probability of being cost-effective than IV-tPA alone at WTP thresholds (Fig. 3).
Budget-impact analysis
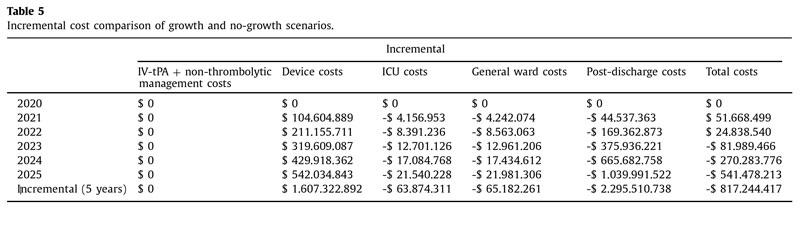
Despite higher per-patient costs in the first and second years, savings began accruing in the third year when MT procedure volume increased (0.96%; AR$8,398,617,43 versus AR$8,480,606,897; (Table 5). Savings increased in the fourth (AR$270,283,776; 2.6%) and fifth years (AR$541,478,213; 4,4%). Over five years, increased MT procedure volume resulted in 1,280 additional patients, at sav- ings of 1.8% (AR$817,244,417) compared to 480 cases at higher costs when volume remained static. Savings are explained by avoided hospitalization and long-term care costs from the third year onward.
Deterministic sensitivity analysis found that the cumulative, in- cremental budget impact over five years was most sensitive to long-term costs for mRS scores of 3 to 5 and the variation of all scores together, followed by mRS scores for non-thrombolytic treatment, mRS scores for MT, and MT cost. Other than variation in long-term cost, all other variables in the analysis tiers maintained savings over the horizon.
Discussion
The purpose of this study was to develop a validated model to estimate the cost-effectiveness and budget impact of IV-tPA and MT for stroke care in Argentina.
According to the base-case model parameters, IV-tPA and MT for treating acute ischemic stroke would save the Argentinian healthcare system money and increase patient utility. IV-tPA and MT were dominant. Results were robust over a wide range of pa- rameters in the deterministic sensitivity analyses, and IV-tPA and MT showed a 100% probability of being cost-effective in the probabilistic sensitivity analyses.
In the scenario analysis, IV-tPA and MT remained dominant (AR$440,669/QALY) with NMB of AR$1,920,639.
Understanding the tradeoffs between short and long-term costs associated with stroke care could be valuable for establishing healthcare policies around stroke in Argentina. A gradual increase in MT yields savings in the short term. Despite the higher up-front costs of treating patients with IV-tPA and MT compared to other alternatives, the superior clinical results of IV-tPA and MT avoid future expenses associated with worse morbidity and disability levels.
The significant clinical efficacy of IV-tPA with MT compared to IV-tPA alone was established in the SWIFT PRIME trial. 13 The study compared global disability at 90 days, according to a 7-point mRS scale, in 196 patients treated with or without MT using the Solitaire device after IV-tPA at 39 centers across North America and Europe. The study found that treatment with MT after IV- tPA reduced global disability at 90 days over the entire range of mRS scores (P < 0.001). Functional independence (mRS 0-2) was reached in 60% of patients in IV-tPA and MT arm, versus 35% in IV-tPA alone (P < 0.001). Data from additional randomized studies and registries (EXTEND-IA in Australia and New Zealand, 7 ES- CAPE in North America, South Korea, Ireland, and the UK, 9 REVASCAT in Spain, 11 MR CLEAN in the Netherlands, 6 and STRATIS in the United States), 12 have supported these findings. Meta-analyses have concluded that MT is safe, highly effective, and reduces disability across a wide range of patient characteristics and geography. 8, 10
The cost-effectiveness of MT has also been evaluated in the UK, 15 Italy, 16 Spain, 14 and Chile. 33 In the UK, treatment with IV- tPA and MT was associated with improved QOL, increased life expectancy, and health status, with overall savings of £33,190 per patient and NMB of £79,402 compared to IV-tPA alone. 15 In Italy, IV-tPA, and MT were cost-effective in the first three years and cost- saving thereafter. 16 In Spain, IV-tPA and MT was associated with a gain of 2.51 QALYs, savings of €44,378, and NMB of €119,744. 14 Finally, in Chile, MT was found to be associated with lower costs, 2.63 incremental QALYs, NMB of $37,289,874 (Chilean Pesos), an ICER of $3,807,413/QALY over a lifetime horizon. 33
Although solid international efficacy and cost-effectiveness evidence of MT exists, its uptake has been slow in Argentina. To our knowledge, the present study is the first to evaluate the cost-effectiveness of MT in this population. Our findings are consistent with studies conducted in other settings.
Limitations
Limitations stem from epidemiological factors inherent to Argentina’s healthcare system. For one, the availability and quality of stroke care at current medical facilities in Argentina vary widely. The government does not require these units in high-complexity centers, and no reliable estimates exist of specialized stroke units throughout the country. 24
Stroke units are mainly concentrated in Buenos Aires and larger provinces. A low prevalence of neurologists in Argentina (2.9 per 10 0,0 0 0 residents) and the heterogeneous geographic distribution complicate consistent delivery of stroke treatment. As demonstrated by the ARENAS registry, these factors contribute to a wide gap between clinical practice guide- lines for stroke and real-world practice in Argentina. 18 Because the institutions that contributed with patient data to this study may be more homogeneous in terms of population, technology adoption, and costs, readers should keep these factors in mind when generalizing our results.
Further, these same factors and others could result in non- compliance with the full SWIFT PRIME inclusion criteria. In the future, it would be of interest to adjust the models using the HERMES collaboration, 10 which pooled patient-level data from the MR CLEAN, ESCAPE, REVASCAT, SWIFT PRIME, and EXTEND IA trials, to improve outcome bias and use of RAPID CT software.
According to the ReNACer registry, 1% of stroke patients accessed thrombolytic therapy in Argentina. 22 Today this rate would be between 4 and 10% according to expert opinion, 34 but still far from European rates. 35 , 36 For this reason, SWIFT PRIME was used as a source of treatment efficacy data, but not for modelling proportions of access to each arm in Argentina. In the BIA, the number and proportions of treatments were proposed based on local data and assumptions validated by local experts.
The same decentralized structure that affects clinical consistency and a lack of national tarifflists might fluctuate costs across providers. Within the same institution, prices are not likely to differ for patients depending on their insurance; however, copay- ments can vary. The deterministic sensitivity analysis corrected for this inter-institution fluctuation.
The utilization of SWIFT PRIME data introduced parametrical uncertainty to the model, due to the possible effect of the trial’s early termination on outcome bias. Nonetheless, local data estimates showed that the distribution by gender, age, race, and comorbidities would be similar between the studied populations. Local data also demonstrated similar results for mRS distribution within the six hour treatment window period compared to SWIFT PRIME patients. 37 We conclude that combined therapy with IV-tPA and MT is cost-effective over time for managing acute ischemic stroke due to LVO, compared to IV-tPA alone in Argentina.
Role of the funding source
Medtronic Plc. provided funds for professional medical writing assistance.
Declaration of Competing Interest
PL, JC, and CT declare no conflicts of interest. EA was compensated for working on this study. JV and DP are Medtronic employees.
Acknowledgements
Jeanne McAdara PhD provided professional medical writing assistance, funded by Medtronic.
Supplementary materials
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jstrokecerebrovasdis. 2022.106595 .
References
- Institute for Health Metrics and Evaluation (IHME). Global Data Exchange. Institute for Health Metrics and Evaluation (IHME) Accessed at http://ghdx.healthdata.org/gbd-results-tool
- Christensen MC, Previgliano I, Capparelli FJ, et al. Acute treatment costs of intracerebral
hemorrhage and ischemic stroke in Argentina. Acta Neurol Scand. 2009;119:246–253. - Instituto Nacional de Estadística y Censos. Tercera Encuesta Nacional de Factores de Riesgo de Enfermedades No Transmisibles . Instituto Nacional de Estadística y Censos; 2013 Accessed at https:// cesni-biblioteca.org/ archivos/3ra- encuesta- nacional.pdf .
- Warlow C, Sudlow C, Dennis M, et al. Stroke. Lancet. 2003;362:1211–1224 .
- Rennert RC, Wali AR, Steinberg JA, et al. Epidemiology, natural history, and clinical
presentation of large vessel ischemic stroke. Neurosurgery. 2019;85:S4–S8. - Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20.
- Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–1018.
- Campbell BC, Hill MD, Rubiera M, et al. Safety and efficacy of solitaire stent thrombectomy: individual patient data meta-analysis of randomized trials. Stroke. 2016;47:798–806.
- Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular
treatment of ischemic stroke. N Engl J Med. 2015;372:1019–1030. - Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731.
- Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom
onset in ischemic stroke. N Engl J Med. 2015;372:2296–2306. - Mueller-Kronast NH, Zaidat OO, Froehler MT, et al. Systematic evaluation of patients
treated with neurothrombectomy devices for acute ischemic stroke: primary results of the STRATIS registry. Stroke. 2017;48:2760–2768. - Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372:2285–2295.
- de Andrés-Nogales F, Álvarez M, de Miquel MÁ, et al. Cost-effectiveness of mechanical
thrombectomy using stent retriever after intravenous tissue plasminogen activator compared with intravenous tissue plasminogen activator alone in the treatment of acute ischaemic stroke due to large vessel occlusion in Spain. Eur Stroke J. 2017;2:272–284. - Lobotesis K, Veltkamp R, Carpenter IH, et al. Cost-effectiveness of stent-retriever thrombectomy in combination with IV t-PA compared with IV t-PA alone for acute ischemic stroke in the UK. J Med Econ. 2016;19:785–794.
- Ruggeri M, Basile M, Zini A, et al. Cost-effectiveness analysis of mechanical thrombectomy with stent retriever in the treatment of acute ischemic stroke in Italy. J Med Econ. 2018;21:902–911.
- Ameriso SF, Gomez-Schneider MM, Hawkes MA, et al. Prevalence of stroke in Argentina: a door-to-door population-based study (EstEPA). Int J Stroke. 2021;16: 280–287.
- Atallah A, Fustinoni O, Zurru M. et al. Identifying barriers in acute stroke therapy in Argentina. ARENAS registry (P2. 014). 2014
- Bahit MC, Coppola ML, Riccio PM, et al. First-ever stroke and transient ischemic attack incidence and 30-day case-fatality rates in a population-based study in Argentina. Stroke . 2016; 47: 1640–1642.
- Insaurralde W, Heuer L, Veronesi C, et al. Accidente cerebrovascular (ACV): estudio
epidemiológico prospectivo en el Hospital SAMIC Eldorado, Misiones, Argentina.
Rev. Argent. Med . 2016; 4: 164–168. - Melcon CM, Melcon MO. Prevalence of stroke in an Argentine community. Neuroepidemiology. 2006;27:81–88.
- Sposato LA, Esnaola MM, Zamora R, et al. Quality of ischemic stroke care in emerging countries: the Argentinian National Stroke Registry (ReNACer). Stroke. 2008; 39:3036–3041.
- Atallah AM, Zurrú MC, Alonzo C, et al. Consenso de diagnóstico y tratamiento agudo del accidente cerebrovascular isquémico consejo de stroke: sociedad Argentina de cardiología. Rev. Argent. Cardiol. 2012; 80: 394 – 410.
- Pigretti SG, Alet MJ, Mamani CE, et al. Consensus on acute ischemic stroke. Medicina. 2019;79(2): 1–46 (Bs. As.)Suppl.
- Ferrante D. Costo-efectividad del Dabigatrán en la prevención de accidente cerebrovascular en la fibrilación auricular en la Argentina. Hematología. 2013;17:115–121.
- Giorgi MA, Caroli C, Giglio ND, et al. Estimation of the cost-effectiveness of apixaban versus vitamin K antagonists in the management of atrial fibrillationn Argentina. Health Econ. Rev. 2015;5:52.
- Briggs A, Sculpher M. An introduction to Markov modelling for economic evaluation.
Pharmacoeconomics. 1998;13:397–409. - Mohan KM, Wolfe CD, Rudd AG, et al. Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke. 2011;42:1489–1494.
- Jung S, Mono ML, Fischer U, et al. Three-month and long-term outcomes and their predictors in acute basilar artery occlusion treated with intra-arterial thrombolysis. Stroke . 2011;42:1946–1951.
- Luengo-Fernandez R, Paul NL, Gray AM, et al. Population-based study of disabilitand institutionalization after transient ischemic attack and stroke: 10-year results of the Oxford Vascular Study. Stroke . 2013;44:2854–2861.
- Nedeltchev K, Fischer U, Arnold M, et al. Long-term effect of intra-arterial thrombolysis in stroke. Stroke . 20 06;37:30 02–30 07.
- Sullivan SD, Mauskopf JA, Augustovski F, et al. Budget impact analysis-principles of good practice: report of the ISPOR 2012 budget impact analysis good practice II task force. Value Health . 2014;17:5–14.
- Lenz-Alcayaga R, Paredes-Fernández D, Hernández-Sánchez K, et al. Cost-utility analysis: Mechanical thrombectomy plus thrombolysis in ischemic stroke due to large vessel occlusion in the public sector in Chile. Medwave . 2021;21:e8152.
- Alet M, Pigretti S, Ciardi C. Comunicación breve: encuesta nacional sobre el tratamiento de reperfusión del accidente cerebrovascular isquémico agudo. Neurol Argent . 2021;13:175–180.
- de Los Ríos la Rosa F, Khoury J, Kissela BM, et al. Eligibility for intravenous recombinant tissue-type plasminogen activator within a population: the effect of the European Cooperative Acute Stroke Study (ECASS) III trial. Stroke. 2012;43:1591–1595.
- Ganesalingam J, Pizzo E, Morris S, et al. Cost-utility analysis of mechanical thrombectomy using stent retrievers in acute ischemic stroke. Stroke. 2015;46:2591–2598.
- Cirio JJ, Ciardi C, Vila JF, et al. Ataque cerebrovascular isquémico agudo de territorio anterior: tratamiento endovascular. Medicina. 2020;80:211–218 (Buenos Aires).